Ariel Pablos-Méndez
President Barack Obama has set forth a vision to realize one of the greatest contributions to human progress: the elimination of extreme poverty. The protection of human life and health is a key component of this vision.
Developing countries are now experiencing an economic transition of health, driven by economic growth, trends in health spending and the changing role of official development assistance. Because of this promising transition, we have a first-ever opportunity to work with these countries to build effective, efficient and equitable health systems with financing approaches that protect people from extreme poverty. Health coverage that ensures universal, equitable access to affordable, quality health services will be an essential ingredient to ending extreme poverty by 2030.1
Big returns on investment
According to the 2013 Lancet Commission on Investing in Health report, financing health services to reduce mortality will play a critical role in ending poverty. The Lancet Commission, co-chaired by Larry Summers and Dean Jamison, noted that reductions in mortality account for 11 percent to 24 percent of recent economic growth in low- and middle-income countries. If we invest an additional $24-$61 billion ($13-$26 per person) annually in health services in low- and middle-income countries, 169 million lives will be saved by 2035, and enhanced financing for health services will result in income returns that are 9 to 20 times the original investment (Figure 1).2
Figure 1: Scaling-up to Grand Convergence & UHC
| Annual incremental lives saved (2035) | Annual incremental cost* (2015–2035) | Proportion of real GDP growth by (2035) | |
|---|---|---|---|
|
Low-Income Countries |
7.4M |
$23B–27B |
3% |
|
Low- and Middle-Income Countries |
7.4M |
$38B–53B |
<1% |
| *Approximately half the investment is in health systems | |||
|
Sources: The Lancet Commission Investing in Health; World Development Indicators |
|||
These investments make a grand convergence in life expectancy between rich and poor countries a feasible goal for our generation. Adults and children living longer, healthier lives become robust contributors to income growth. The impact of improved health outcomes on a country’s economic productivity plays a vital role in ending extreme poverty.
Investments in health by USAID and our partners have produced concrete results. Over the past 50 years, infant and child death rates in the developing world have fallen by 70 percent. Deaths of children under 5 decreased from 7.7 million in 1990 to 4.8 million in 2011 in the 24 priority countries of USAID’s Ending Preventable Child and Maternal Deaths initiative.3 In countries with efforts focused on maternal and child health, the maternal mortality ratio decreased by more than half, from 695 deaths per 100,000 women in 1990 to 315 per 100,000 in 2010.4
From 2005 to 2011, in conjunction with USAID’s work toward an AIDS-free generation, deaths due to AIDS-related causes fell 25 percent. In sub-Saharan Africa, the number of AIDS-related deaths declined by nearly one-third. Furthermore, over 46.5 million people received HIV testing and counseling through the U.S. President’s Emergency Plan for AIDS Relief, including 11 million pregnant women.5
Economic transition in health
What do we mean by an economic transition in health? This transition occurs when developing countries, through economic growth and associated increases in total health expenditures, reach a point where they can fund an essential package of cost-effective public health services and clinical health services and support health systems that are capable of substantially reducing the country’s disease burden through domestic resources alone.
As many low-income countries experience rapid growth, their total health expenditures grow as well, putting essential health services within reach for entire populations. Countries that reach this economic transition point are able to use their newly available domestic resources to provide everyone with access to health care, including people in extreme poverty.
Concurrently, it’s becoming more affordable to ensure these essential health services. In 2014, the World Health Organization’s Commission on Macroeconomics and Health estimated a $51 cost per capita for its essential package of health care services—which includes clinical and public health interventions in tuberculosis, malaria, HIV and maternal and child health. Also in 2014, the International Health Partnership High Level Task Force on Innovative Financing of Health Systems estimated a $71 per capita cost for its essential package of health services.6
In some developing countries, the challenge is not affordability but how the newly available domestic resources are spent, namely how to shift health care financing away from a status quo that largely involves out-of-pocket payments by people when they need services.
Without equitable health financing, countries are likely to experience the high out-of-pocket spending associated with the growth of unregulated private providers and the inadequate delivery of public services, leading many people into ill health and poverty. High out-of-pocket spending is associated with catastrophic health spending, impoverishment and underutilization of essential services, such as immunizations, by the poor. Countries worldwide recognize the need to decrease their reliance on out-of-pocket payments at the point of service delivery.
According to a comprehensive analysis of surveys from 89 countries, around 150 million people each year suffer financial catastrophe; 100 million are pushed to live below the poverty level because they need to pay for health services. More than 90 percent of the people pushed into poverty by health spending live in low-income countries.7
Unfortunately, a problematic “financing ditch” can occur as countries begin to move out of low-income country-status (Figure 2). Official development assistance providers often respond to the new prosperity by cutting aid. However, the country’s public sector does not quickly or automatically fill the gap.
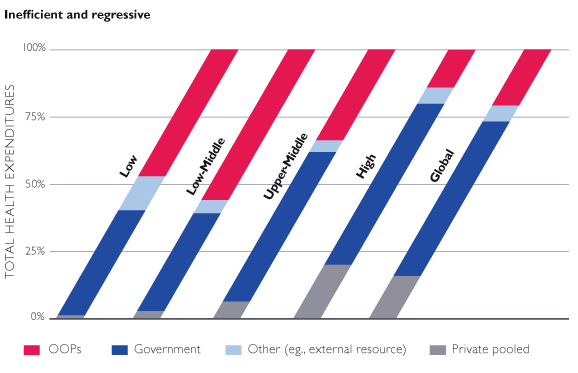
Instead, households are forced to compensate, often through out-of-pocket spending or by missing out on lifesaving services. Sustainable emergence from poverty is a complicated picture. One key solution is: Proactively pool risks through equitable financing arrangements for health.
Universal health coverage— the new frontier
Universal health coverage has been defined as a condition where all of the people who need health services—including health prevention, promotion, treatment, rehabilitation and palliative care— receive them without undue financial hardship,8 and countries are adapting diverse approaches to achieving it. Some nations use a national insurance system that buys services from both private and public providers. Others use the public delivery system to provide better access to health services.9
Over the past decade, there has been growing evidence of developing countries with relatively low incomes improving their health financing arrangements, thereby improving health coverage with essential services and protecting people from impoverishment. Countries as diverse as Colombia, Chile, Ghana and Thailand have introduced such health-financing arrangements.
In Thailand, after a universal health coverage scheme was introduced in 2002, health care usage rates improved, equity of usage increased and the incidence of impoverishing health expenditures declined.10 The number of households pushed under Thailand’s national poverty line as a result of out-of-pocket spending fell from 120,000 in 2002 to 40,000 in 2009.11
The Parliament of Ghana, in an effort to reduce the very heavy burden of out-of-pocket payments, passed the National Health Insurance Law in 2003, requiring that all citizens enroll in government- sponsored district health insurance schemes. Seventy to 75 percent of the funds for this insurance program comes from the value-added tax on goods; an additional 20 to 25 percent of the funding comes from Social Security and National Insurance Trust contributions by workers in the formal public and private sectors. Finally, direct premiums from workers account for approximately 5 percent of the financing. Indigents, minors under age 18, the elderly over age 70 and all pregnant women are covered and exempted from premium payments. Most outpatient and inpatient care services are covered.12 As of 2008, 12 million people out of a total population of 21 million, or 61 percent of the population, were insured.13
Universal health coverage implies equity of access for all, including those living in extreme poverty who may be unable to pay for out-of-pocket costs or make payments to prepaid or pooled health insurance arrangements. Equitable access is critical for the extremely poor, who typically forgo even essential health care. This under-utilization of essential services by the poor leads to an ongoing cycle of poverty, as people who are sick and vulnerable are unable to participate in the labor market.
Out-of-pocket costs should be zero for the poor, and coverage should focus first on services for conditions that typically affect the poor, such as infectious diseases.14 When the Government of Ethiopia introduced a health extension program in 2003 in certain regions, a first step toward universal coverage of primary care, the program focused first on conditions that disproportionally affect the poor. Today it is fully integrated into the broader health system and provides 16 defined packages of essential health services. All health extension program services are free and available to everyone.15
Universal health coverage is the new frontier in global health. As countries continue to evolve, official donors will shift from providing commodities and services directly to countries and beneficiaries to strengthening health and finance systems in low- and middle-income countries. This shift will occur as some countries graduate from reliance on foreign assistance, instead generating domestic income to finance health expenditures. Ultimately, improving domestic resources for universal health coverage, which includes spearheading tax administration and policy changes, is the path that will sustain viable health systems in developing countries.
Not all low-income countries will travel this path toward self-sufficiency expeditiously. Some rapidly growing economies will be starting from such a low base that they will be unlikely to generate enough domestic revenue to fully pay for health. These countries will continue to need aid to achieve critical health goals.
Pioneering new health financing
In the face of this evolving economic transition in health and current patterns of high out-of-pocket spending on health, what should we do to help poor people get the health services we know they need to thrive? I believe we should continue to embrace the challenge of working with developing countries to harness their growing prosperity to fundamentally shape the future of health financing and universal health coverage.
USAID investments in global health in particular can support President Obama’s vision of ending extreme poverty because they involve:
- Collaboration with countries on mobilizing emerging domestic resources to empower them to face the inevitable insufficiency and fluctuations of official development assistance. As part of achieving our goals for an AIDS-free generation, for example, USAID has been increasing country capacity to self-finance and sustain HIV epidemic control efforts.
- Expertise working at the intersection of health and finance, gathered from over 50 years’ experience applying integrated, sustainable solutions to individual country contexts. As our development partner countries face enormous struggles unique to the current transition period, we understand our responsibility to work with them to recalibrate the mix of official development assistance and domestic resources for health.
- Experience by the U.S. Government homing in on two primary health goals: ending preventable child and maternal deaths by 2035 and ensuring an AIDS-free generation. This work with low- and middle-income countries on health systems and finance gives us the ability to help these countries guarantee adequate focus on essential services related to these goals.
USAID historically has taken a leadership role in helping eliminate extreme poverty through global health programs that address diverse diseases and complicated public health challenges. Since 2010, for example, USAID nutrition programs have reached more than 46 million children under the age of 5, including 12.5 million in FY 2013.16
From 1990 to 2012, there has been a 72- percent reduction in the risk of a child dying from pneumonia or diarrhea, from 50 per 1,000 to 14 per 1,000. USAID’s health programs ensured the safety of drinking water; in 2013 they supported the treatment of 3.2 billion liters, enough for over 4 million people. Additionally, USAID supported the introduction of vaccines against rotavirus and pneumococcus, two of the leading disease agents for diarrhea and pneumonia, and provided low-cost treatment in more than 1.8 million cases. 17
Under the President’s Malaria Initiative, in FY 2013, USAID protected over 45 million people from malaria with some type of prevention measure.18 Deaths from tuberculosis have decreased 41 percent since 1990, and the overall prevalence of tuberculosis reduced 40 percent in USAID-supported programs. USAID’s support for neglected tropical diseases since 2006 has expanded to reach 25 countries, leveraging a total of $6.7 billion in donated medicines from a $386-million investment.19
Overall, USAID’s health-sector work contributes to efforts that ensure that poor and vulnerable people can survive and join the labor force as productive contributors. These efforts catapult poor countries toward unprecedented economic growth, making the end of extreme poverty possible. With our partners, USAID is stressing the imperative of health policy reform to prioritize customized strategies and institutional arrangements that increase domestic financing, improve value for money and ensure fair, sustainable universal health coverage.20 With these actions, I believe all USAID global health programs will be key to dramatically increasing the number of people in developing countries who are able to avoid living in extreme poverty.
Ariel Pablos-Méndez is the assistant administrator for Global Health at USAID.
1 World Bank, “Universal Health Coverage for Inclusive and Sustainable Development—A Synthesis of 11 Country Case Studies.” (April 11, 2014).
2 The Lancet Commission on Investing in Health, Global Health 2035: A World Converging Within a Generation. (December 2013); Global Health 2035—Supplementary Web Appendices, www.globalhealth2035.org (June 2014).
3 USAID, Fifty Years of Global Health, Saving Lives and Building Futures—USAID’s Tradition Continues. (2014).
4 USAID Annual Progress Report to Congress: Global Health Programs FY 2013.
5 USAID, Fifty Years of Global Health, Saving Lives and Building Futures—USAID’s Tradition Continues. (2014).
6 These 2014 cost calculations for the two different packages of essential services assume an inflation rate of 2.5 percent annually for the CMH package and 3.5 percent annually for the TFIF package (using medium costing scenario for the TFIF package).
7 Ke Xu, David B. Evans, Guido Carrin, Ana Mylena Aguilar-Rivera, Philip Musgrove and Timothy Evans, “Protecting Households from Catastrophic Health Spending,” Health Affairs. Vol. 26, no.4 (2007).
8 WHO (World Health Organization), The World Health Report— Health Systems Financing: The Path to Universal Coverage. http://www.who.int/whr/en/index.html. 2010.
9 World Bank, Universal Health Coverage for Inclusive and Sustainable Development—A Synthesis of 11 Country Case Studies. (April 21, 2014).
10 Final report of the Centre on Global Health Security Working Group on Health Financing, “Shared Responsibilities for Health—A Coherent Global Framework for Health Financing.” May 2014.
11 Thailand’s Universal Coverage Scheme: Achievements and Challenges: An Independent Assessment of the First 10 Years (2001-2010) (2012), Nonthaburi: Health Insurance System Research Office.
12 African Health Economic Association Conference on Towards Universal Health Coverage in Africa—Key Issues. http://afhea.org/ conference/conference2011/files/Key-Issues.pdf (2011). 13 Joint Learning Network for Universal Health Coverage, www.jointlearningnetwork.org (June 2014).
14 Final report of the Centre on Global Health Security Working Group on Health Financing, “Shared Responsibilities for Health—A Coherent Global Framework for Health Financing.” May 2014.
15 World Bank, Universal Health Coverage for Inclusive and Sustainable Development—A Synthesis of 11 Country Case Studies. (April 21, 2014).
16 USAID Annual Progress Report to Congress: Global Health Programs Fiscal Year 2013.
17 Ibid.
18 Ibid.
19 Ibid.
20 Ariel Pablos-Méndez, Caroline Ly, Allyla Nandakumar, Timothy Evans, Patrick Eozenou, Olusoji Adeyi, “The Economic Transition of Health in Africa: A Call for Progressive Pragmatism.” Oxford Handbook on Africa and Economics. (March 13, 2014).
Frontiers in Development
Section 4: Going Forward (Without Going Backward)







Comment
Make a general inquiry or suggest an improvement.