- What We Do
- Agriculture and Food Security
- Democracy, Human Rights and Governance
- Economic Growth and Trade
- Education
- Ending Extreme Poverty
- Environment and Global Climate Change
- Gender Equality and Women's Empowerment
- Global Health
- Water and Sanitation
- Working in Crises and Conflict
- U.S. Global Development Lab

At a Glance
- Introduction
- Why Do Behaviors Matter for Nutrition?
- How Do Behaviors Change?
- How Are Behaviors Identified?
- Key Considerations for Nutrition SBCC Design
- Key Considerations for Nutrition SBCC Implementation, Monitoring, and Evaluation
- Advancing the Strategic Agenda for At-scale Nutrition SBCC
- Summary
- Additional Resources
- References
- Footnotes
View the PDF [PDF, 585KB].
Introduction
Box 1. What Is Nutrition SBCC?
Nutrition SBCC is a set of interventions that systematically combines elements of interpersonal communication, social change and community mobilization activities, mass media, and advocacy to support individuals, families, communities, institutions, and countries in adopting and maintaining high-impact nutrition-specific and nutrition-sensitive behaviors or practices. Effective nutrition SBCC leverages enablers of behaviors and reduces barriers to adopting and maintaining behaviors over time.
This technical guidance brief is based on the understanding that human behavior is complex and profoundly influenced by social norms, access to resources, self-efficacy, structural constraints and opportunities, and habits. Systematically addressing the range of behaviors that have a direct or indirect impact on nutrition as well as the social and environmental factors that influence the adoption and maintenance of these behaviors is critical to the implementation of the Multi-Sectoral Nutrition Strategy for 2014–2025 (USAID, 2014). In fact, four of the outcome-level indicators outlined in the strategy (p. 355) are largely behavioral,1 and the other two are directly influenced by behavior.2
Social and behavior change (SBC) programming has long been an area of strategic priority for the U.S. Agency for International Development (USAID). The Agency has invested heavily in social and behavior change communication (SBCC), an important SBC approach, for more than 3 decades, and it remains one of the world's leading funders of SBCC research and programming. Recently, USAID has been investing more in interventions that strengthen integration between both communication-focused and other SBC approaches. While USAID recognizes SBCC as one of the cornerstones of its nutrition investments (see Box 1), it also promotes the use of structural, socioeconomic, and environmental interventions that reduce barriers to and build on enablers for change.
Successfully influencing human behavior requires an understanding of how behaviors change. This brief summarizes key considerations and provides links to available resources and useful tools for USAID Missions and implementing partners to design, implement, monitor, and evaluate nutrition SBCC interventions.
Why Do Behaviors Matter for Nutrition?
The United Nations Children's Fund (UNICEF) conceptual framework on nutrition, developed more than 25 years ago, focuses on three underlying causes of undernutrition: (1) inadequate care and feeding practices, (2) household food insecurity, and (3) an unhealthy household environment and inadequate health services (1990). Interventions that address these underlying conditions, related behaviors, and the broader enabling environment are defined as nutrition-sensitive. The immediate conditions for optimal nutrition are adequate dietary intake and low disease burden; interventions that address these immediate causes and related behaviors are defined as nutrition-specific.
Virtually all the immediate and underlying causes of malnutrition are behavioral – influenced by the behaviors of individuals and their household members. Nutrition is also influenced, however, by the behaviors of many other actors. These actors range from healthcare providers and school teachers to farmers and other agricultural agents, from religious and community leaders to private sector companies and policymakers, who collectively directly or indirectly influence care and feeding practices, household food security, the household environment, and healthcare services.
How Do Behaviors Change?
Figure 1. The Socio-Ecological Model for Change

In this section, we summarize key principles in designing effective, at-scale SBCC interventions. They are grounded in evidence about why people act as they do – from public health; social sciences, including psychology; behavioral and traditional economics, and sociology; and marketing and communication sciences. These principles have guided effective SBCC intervention design for increasing the uptake of individual and group behaviors across multiple sectors.3
Individuals usually act in the context of families, communities, and countries. Their behaviors are influenced directly and indirectly by their social and economic groups, their physical environment, the market environment, and the public and private services and policies that guide them. The socio-ecological model, which is often used to illustrate aspects of context (see Figure 1), is viewed as one of the most relevant to nutrition SBCC. The model demonstrates how effective SBCC interventions can simultaneously facilitate change in the social, physical, market, and policy environments to enable individuals to adopt and maintain the behaviors being promoted. Given the diversity of influencing factors, behaviors should be promoted through multiple approaches, for multiple influencers, and at multiple contact points (e.g., family members, peers, health workers).
To adopt and maintain a given behavior, most individuals need more than information. To have the ability to act, they may need access, motivation, encouragement, confidence, and/or support. Depending on the behavior, a shift in social norms may be required. Individuals act according to culturally influenced identities, hierarchies, and socially accepted norms. Recent evidence reinforces the notion that social support, perceived and actual, is often key to trying and sustaining behavioral changes (World Bank, 2015). It is critical to acknowledge that even with information, motivation, and supportive social norms, individuals may not be able to adopt and maintain behaviors without the required skills, self-efficacy, access to services, and access to nutrition-related resources (e.g., food, supplements, soap, seeds).
Many nutrition behaviors are habitual, so interventions may need to disrupt current habits and establish new ones. Recent evidence from behavioral economics shows that individuals are more likely to make a change in behavior if the change fits their "existing mental model" and group identity. Mental models and habits often need to be encouraged through changes in the environment and behavioral "nudges" that consciously or subconsciously trigger a desired behavior. For example, farmers may be more likely to buy inputs for the next growing season if these are promoted and made available to them just after the harvest, when they feel more economically secure (World Bank, 2015).
SBCC interventions need to be tailored for different populations. Different groups of individuals, or audiences, within a population are likely to think, feel, and react differently to a given behavior. To the extent possible, projects need to design their SBCC interventions in a way that acknowledges and carefully addresses those differences. For communication interventions, this is commonly referred to as audience segmentation. Interventions need to be designed with the right message for the right person, reaching each at the right time.
How Are Behaviors Identified?
Ideally, behaviors to be promoted by a given project should be decided collaboratively with in-country stakeholders, based on the characteristics of the local context, including cultural barriers and resources, as well as household decision-making structures (see Aubel's World Vision International and Infant & Young Child Nutrition [IYCN] Project reports on involving grandmothers in the Additional Resources section). The SBCC design process, described below, systematically identifies priority behaviors based, in part, on how closely linked a behavior is to a desired outcome and identifies barriers and enablers to people adopting and maintaining the priority behaviors. To identify the most critical behaviors, program designers will need to review the available data, conduct formative research, and analyze the causes of malnutrition in the particular context and for particular populations.
Thanks to decades of systematic evidence building, there is an established evidence base for many nutrition-specific practices, their link to outcomes, and which SBCC interventions have successfully facilitated change in those practices. This base gives program planners a head start in designing nutrition-specific SBCC. An illustrative list of some of these evidence-based behaviors that affect the status of maternal, infant, and young child nutrition (MIYCN) practices are presented in Table 1 (SPRING, 2014a).
|
Table 1. Evidence-Based MIYCN Behaviors |
|
|
Intervention Area |
Illustrative Behaviors |
|
Dietary practices during pregnancy and lactation |
|
|
Breastfeeding practices |
|
|
Complementary feeding practices |
|
|
Control and prevention of anemia |
|
|
WASH-related behaviors |
|
Nutrition-specific and nutrition-sensitive practices are often promoted in the context of wider maternal and child health interventions. Nutrition SBCC designers working in this context can now draw on a list of Accelerator Behaviors, developed by USAID's Preventing Child and Maternal Deaths initiative. The Accelerator Behaviors were developed based on a consultative process that included the Population-Level Behavior Change Evidence Summit for Child Health and Development in June 2013. USAID identified the improved behaviors with the highest impact on rates of mortality reduction. All of these behaviors directly or indirectly impact nutrition during the first 1,000 days, and indeed some of the behaviors are reflective of the high-impact MIYCN practices listed in Table 1. For more information on the Accelerator Behaviors, visit acceleratorbehaviors.org/index.
In addition to Accelerator Behaviors, USAID introduced the idea of Related Behaviors that help improve the enabling environment to support the practice of the Accelerator Behavior. This is similar to the way nutrition-sensitive behaviors increase access to and resources for practicing nutrition-specific behaviors.
Programming experience, evidence of effectiveness, and implementation science are stronger for nutrition-specific behaviors4,5,6 than for nutrition-sensitive behaviors. However, the importance of nutrition-sensitive programming is widely acknowledged. Evidence suggests that SBCC interventions in the following diverse sectors can contribute substantially to improved nutrition outcomes: agriculture and food safety, social safety nets, early childhood development, maternal mental health, women's empowerment, child protection, classroom education, water and sanitation, and health and family planning services (Black et al., 2013).
It is well documented that behaviors related to women's wellbeing – whether nutrition-specific or nutrition-sensitive – have an effect on both maternal and child nutrition (SPRING, 2014b). For example, women's control over household assets and use of income leads to better diets for women and children (Coates & Galante, 2015; Olney et al., 2015). Women are better able to care for themselves and their children (Webb & Kennedy, 2014) when demands on their time and their need to do physical labor are reduced; reducing these demands also improves their and their children's health status (Herforth, Jones, & Pinstrup-Andersen, 2012).
Key Considerations for Nutrition SBCC Design
Nutrition SBCC interventions should not be designed separately from other project interventions. Rather, the design as well as the implementation, monitoring, evaluation, and documentation of SBCC programs should be an integral piece of the overall project design. The best practices that apply to nutrition programming generally also apply to nutrition SBCC.7 Like all nutrition interventions, nutrition SBCC must be designed and implemented with quality, equity, scale, and sustainability in mind.
The nutrition SBCC design process should engage a multidisciplinary team of nutrition, gender, and sectoral technical experts (e.g., water, sanitation and hygiene [WASH]; agriculture; or education); specific SBCC experts (communication and media/materials designers); in-country partners, including public, private, and community stakeholders; and monitoring and evaluation experts.
Several different tools and representations of SBCC design processes can be used when designing nutrition SBCC, some of which are included in the SBCC concepts, models, and strategy design section in Additional Resources. The World Bank has a simple graphic showing the SBCC design, implementation, monitoring and evaluation, and re-design process as a spiral with repeating phases to indicate that effective SBCC work is an iterative process that uses emerging data to learn from and to make mid-course corrections (see Box 2).
Typical steps in the SBCC design process include –
I. Identify behaviors related to project objectives. It is important to begin with evidence-based behaviors related to the project objectives. For example, a project aimed at reducing anemia may logically prioritize the intake of iron supplements or deworming medication.
II. Gather available data, which could include reviewing primary or secondary data and conducting formative research. To identify priority behaviors and appropriate SBCC approaches, program designers will need to understand the causes of malnutrition in the particular context of and for specific populations. This includes a review of interventions currently being implemented in the country or the project context that might directly or indirectly affect nutrition. Formative research (see Box 3) is critical for identifying barriers to and facilitators of key behaviors, designing the overall strategy, and developing messages, when appropriate, which resonate both with the priority and/or influencing group(s) and effectively address the identified issues. Formative research can also help identify and build on existing positive behaviors to advance the SBCC approaches. It is important to focus or refocus limited SBCC budgets on behaviors that have the greatest potential for contributing to positive nutrition outcomes for the priority group(s). Data collection, as well as analysis, should be done in consultation with target groups and other local and national stakeholders.
Box 2. Understanding Behavior and Identifying Effective Interventions
Are Complex and Iterative Processes
As SBCC is an approach that incorporates the psychological and social aspects of decision-making, the intervention cycle looks different than other approaches. The resources devoted to definition and diagnosis, as well as to design, need to be larger than programming approaches that do not vary as much based on the target audience. The implementation period tests several interventions, each based on different assumptions about choice and behavior. One of the interventions is adapted and fed into a new round of definition, diagnosis, design, implementation, and testing. The process of refinement continues after the intervention is scaled up.
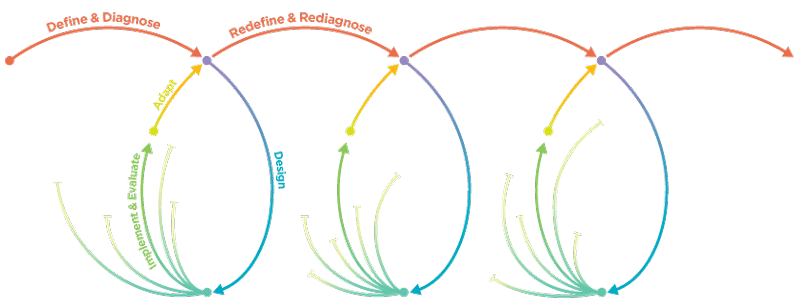
Source: World Bank. (2015). World development report 2015: mind, society, and behavior." p.21. Washington, DC: World Bank. Available at www.worldbank.org/en/publication/wdr2015
III. Design an SBCC strategy using primary or secondary data, findings from formative research, experience, and logic to –
Box 3: Formative Research
Formative research to inform the design of SBCC interventions is critical to the success of nutrition projects, as well as projects designed to achieve nutrition-related outcomes. Which nutrition behaviors to promote, and the specific barriers to and enablers for those behaviors among different population groups, are all highly context specific. They vary according to cultural, geographic, social, economic, and other family and community factors. In a project context, formative research is the key to understanding –
- what motivates or inhibits the optimal practice of the most critical (often least practiced) behaviors among priority groups
- perceptions about these practices
- possible ways to facilitate new or improve current practices
Many materials and documents are available on nutrition-related formative research methods (see Additional Resources).
A. Define and prioritize behaviors that will be promoted. Evidence confirms that SBCC interventions are most effective when they promote a limited number of "doable" actions at one time. For example, in an area where caregivers commonly provide water to infants, a project may focus on encouraging mothers not to give water to a baby in the first 6 months as part of promoting the practice of exclusive breastfeeding to 6 months of age. Behaviors should have a substantial impact on achieving the project objectives, contribute to nutrition-specific or nutrition-sensitive outcomes, and be feasible for the priority groups to adopt and maintain in the current context and with the current resources.8 Nutrition SBCC program design should realistically reflect the budget, timeframe, and human resources available to promote all the proposed practices strategically and coherently.
B. Consider and plan how the proposed interventions will bring about sustained changes in priority behaviors. This may be a theory of change or a results framework, but it should present the development hypothesis of how activities will lead to outputs, outcomes, and, eventually, impacts. The theory of change or results framework should inform a program monitoring plan that includes specific, measurable, achievable, relevant, and time-bound (SMART) indicators of the inputs, processes, outputs, outcomes, and impacts identified.
C. Refine the focus on target populations, including the priority group(s), or the population expected to adopt and maintain the priority behaviors, and the influencing groups depicted in the socio-ecological model, such as partners, families, peers, leaders, service providers, private sector, non-governmental organizations, and government representatives.
D. Select the best available approaches, channels, or delivery platforms and the best methods, media, and materials for reaching the proposed target population(s). See some resources for this selection process in the Additional Resources section.
E. Consider whether communication-focused and other activities are both being used to reduce barriers and build on enablers for action. Most effective SBCC strategies include a mix of communication-focused and other activities, such as –
- interpersonal communication, including – but not limited to – facility-based counseling, home visits, and support groups
- community mobilization, including fairs, contests, and dialogues as well as community radio and video production and dissemination events
- social marketing of technologies or commodities (e.g., home water treatment, fortified foods)
- mass media campaigns (e.g., television dramas, radio broadcasts)
- systems strengthening – improving access to and quality of goods and services (e.g., training of health workers on improved nutrition counseling skills and behaviors)
- behavioral economics – using conscious and unconscious factors that drive decisions and actions to make optimal behaviors easy and desirable
- the creation of social, policy, or financial incentives or disincentives to behavior change
- advocacy conducted at the community level and reaching up to the national level, among decision-makers and policymakers
Some activities should reach the priority groups while others should reach the influencing groups, whose support for the behavior is critical. If social, economic, political, or physical barriers are identified, behaviors are unlikely to change unless structural interventions are taken to reduce those barriers, regardless of how well the communication activities have been designed. For example, food-insecure households may need social protection interventions as well as nutrition SBCC to improve maternal diets and child feeding practices; or households may need support to access seeds and other inputs for improved household gardens.
Key Considerations for Nutrition SBCC Implementation, Monitoring, and Evaluation
The various elements of implementation and monitoring and evaluation (M&E) of nutrition SBCC interventions should be embedded in the overall implementation, design, quality assurance, and M&E plans of a given project because they are integral to the success of the program. The initial program design should be informed by data about priority practices related to objectives and by potential barriers and enablers in a given context among different populations. Initial insights about behaviors, barriers, and enablers as well as a plan and budget for SBCC design – including formative research, media and materials design, implementation, and M&E activities – should be included from the procurement phase on, refined during program start-up, and updated over the course of a program. Ideally, SBCC technical expertise will be available within implementing partners as key personnel as well as within host governments.
Implementation
Best practices in program implementation generally also apply to nutrition SBCC. Program managers should develop a detailed implementation plan and a realistic budget for SBCC-related activities. A particular challenge for SBCC implementation results when data from formative research are translated into appropriate and actionable SBCC activities. Sometimes, this means that implementers need to do things differently – for example, prioritizing some behaviors to promote first and, later in the project, bringing in other behaviors or other priority groups; or being flexible to change interventions if barriers are not being reduced or behaviors are not changing as expected in the initial design.9
Managers, staff, and partners should update and use implementation plans to track progress and budgets throughout the life of the project. An essential part of implementation is the iterative process of program design. Projects need to be flexible enough to make periodic or midcourse corrections and to redesign future interventions based on careful, regular monitoring of quality data or evidence of impact.
Monitoring and Evaluation
Indicators related to nutrition SBCC should be included in the overall project M&E plan. Ideally, the M&E plan should be based on an explicit theory of change – in other words, how activities will lead to outputs, outcomes, and, eventually, impacts. It should include indicators of the inputs, processes, outputs, outcomes, and impacts identified. The information gathered through monitoring activities should help implementers identify interventions or aspects of interventions that are not working as planned, to then make periodic or midcourse corrections, as described earlier, as the iterative process of SBCC implementation. Nutrition SBCC M&E should measure whether –
- priority and influencing groups are being reached with interventions
- interventions are being implemented consistently and with good quality
- media/materials are designed, field tested, produced, and used as intended
- goods and services needed to perform behaviors are accessible and of good quality
- barriers are being reduced and enablers strengthened through communication and structural interventions as planned
- changes in the enabling environment are occurring as planned (e.g., social norms, local markets, support from leaders)
- target populations are adopting the behaviors
The use of standardized indicators can make data more comparable across projects (nationally and globally) to identify determinants of effectiveness at-scale in different contexts and for different types of behaviors. Performance monitoring plans must be feasible to implement and provide useful, relevant information for donors, implementers, and partners, including communities and other local stakeholders. An important, but often forgotten, piece of M&E is the documentation and dissemination of findings.
As with other nutrition efforts, adequate time and money for effective knowledge management, including the documentation and dissemination of results or findings, products, tools, challenges, successes, and lessons learned, is a critical step in programming. A recent systematic literature review (see Additional Resources) revealed a striking lack of information about the actual implementation details and the challenges faced.
Advancing the Strategic Agenda for At-scale Nutrition SBCC
Within the context of the most recent global evidence validating SBCC theories and approaches, a Strategic Agenda for At-Scale Nutrition SBCC emerged from a systematic process supported by USAID in 201410 (SPRING, 2015). A blueprint was developed for program planners and implementing partners committed to creating lasting, at-scale SBCC components of nutrition programs to drive the social and individual behavior changes needed to meet global and country-level nutrition commitments. Given the inclusion of SBCC as a key activity in its Multi-Sectoral Nutrition Strategy, USAID and its partners now have a clear opportunity to advance this Strategic Agenda. Stakeholders include all development sectors engaged in driving nutrition outcomes and the associated decision-makers, program planners, designers, practitioners, and influencers. The MSNS also presents opportunities for working with new kinds of partners to leverage resources and expertise to facilitate social and behavior change. The cumulative SBCC efforts of multiple actors should lead to substantial improvements in global nutrition. The strategic agenda focuses on several interrelated categories of actions to advance the impact of future investments in nutrition SBCC.
Promoting scale-focused nutrition SBCC
- Ensure that SBCC is an integral component of every nutrition intervention in every sector
- Invest only in pilots with a clear potential for scale
- Implement approaches that enable short-term behavior change along with the longer-term structural changes needed for sustainability
- Leverage resources and opportunities to build on existing systems (formal and informal)
Driving excellence in design and implementation
- Use iterative implementation approaches where ideas and insights are constantly tested and adapted
- Focus on a limited number of behaviors; think of phased and cumulative interventions
- Cut through crowded information environments to connect with clients and audiences
- Involve community members in leading and evaluating community-based programs
Building on the existing evidence base for SBCC's impact on nutrition
- Use standard indicators to measure social change, behavior change, and outcomes
- Align program reporting requirements to include common aspects of design and implementation
- Identify key success factors for replicating or scaling up interventions
- Compare the cost effectiveness of approaches and communication channels, alone or in combination, at different scales
Summary
This brief makes a case for increased emphasis on effective, at-scale SBCC to achieve the objectives of the Multi-Sectoral Nutrition Strategy and to improve nutrition globally. It also includes introductory guidance for designing, implementing, monitoring, and evaluating SBCC interventions. Readers are encouraged to use the Additional Resources in this brief to help realize the potential of at-scale SBCC for creating lasting changes in nutrition.
SBCC Design Case Study: Exclusive Breastfeeding in Ethiopia
A project in rural Ethiopia worked with local pastoralist communities and households to increase the rates of exclusive breastfeeding (EBF). Project staff, primarily urban Ethiopians, were convinced that the reasons women did not exclusively breastfeed were because –
- They had to leave their babies at home to tend to their herds.
- Husbands pressured them to stop breastfeeding early due to cultural prohibitions against sex during the breastfeeding period.
The project conducted formative research with representative groups of mothers, fathers, and older women to explore these issues. People were very open about the "sex taboo," saying that only one clan believed this, and the belief was changing in that clan. They also said women usually took small babies with them to tend herds or other family members did the work.
The main barrier to EBF that all groups identified was concern about the impact of EBF on mothers. The community linked mothers' feeling tired and dizzy – symptoms of dehydration and anemia – with EBF.
The project then conducted Trials of Improved Practices (TIPS), another formative research method, which works through a participatory negotiation process with families to identify "small, doable" actions to help mothers feel healthier, more energetic, and supported. Families found they were able to support mothers in drinking an extra cup of milk every day, eating an egg 3 or 4 days a week, drinking clean water whenever they were breastfeeding, and sitting comfortably with their back supported when they were breastfeeding. Fathers were encouraged to be "hero fathers" by making sure they gave mothers the milk and eggs, or money to buy them, and to help them remember about drinking safe water and sitting comfortably when breastfeeding. The ideal of hero fathers already existed in the community, and one reason for the SBCC campaign effectiveness is that it persuaded them that these new behaviors fit with men's aspirations to be hero fathers.
Mothers reported feeling much better after incorporating these practices into their routine, and families and communities became convinced when they also saw the improved livelihood and health status of their EBF babies.
This approach also required changes in project staff attitudes and behaviors. While the SBCC intervention to promote the small, doable actions identified through the formative research was being designed, project staff kept focusing on mothers leaving their babies at home and the "sex taboo". This was, in part, because sex was viewed as a more interesting topic to explore than anemia. The SBCC team had to remind them many times that these were not the barriers identified by the community members. Eventually, the project staff bought into the idea of instead focusing on the barriers identified by community members, and the SBCC interventions moved ahead with newfound focus on how to help mothers feel better to improve EBF practices.
This technical brief will be periodically updated. Comments from readers are welcome to Leslie Koo, especially those that clarify the information provided or indicate where additional information would be useful. (Last updated July 2017)
Additional Resources
SBCC Concepts, Models, and Strategy Design
Alive & Thrive. Interpersonal communication and community mobilization: Featured tools.
Alive & Thrive. Mass communication: Featured tools.
Aubel, J. (2014). Involving grandmothers to promote child nutrition, health and development: a guide for programme planners and managers. Uxbridge, UK: World Vision International.
Health Communication Capacity Collaborative (HC3). How to develop a channel mix plan..
HC3. How to design SBCC messages.
Ivankovich, M. B., & T. Faramand. (2015). Enhancing nutrition and food security during the first 1,000 days through gender-sensitive social and behavior change: a technical brief [PDF, 992KB]. Washington, DC: CORE Group.
Infant & Young Child Nutrition (IYCN) Project. (2011). The roles and influence of grandmothers and men: evidence supporting a family-focused approach to optimal infant and young child nutrition. Washington, DC: USAID.
Johns Hopkins Bloomberg School of Public Health Center for Communication Programs. (2014). The P process: five steps to strategic communication. Health Communication Capacity Collaborative. Baltimore: Johns Hopkins Bloomberg School of Public Health."The P Process" is a tool that walks the user through a step-by-step approach to strategic communication from analysis through design, development, implementation, and evaluation .
Michie, S., van Stralen, M. M., & West, R. (2011). The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implementation Science 6:42.
Technical and Operational Performance Support (TOPS). (2013). Designing for behavior change: for agriculture, natural resource management, health and nutrition. Washington, DC: TOPS. Six-day training curriculum for community development program managers and planners.
Guides for Designing, Conducting, and Analyzing Results of Formative and Consultative Research
Cooperative for Assistance and Relief Everywhere (CARE). (2013). Formative research: A guide to support the collection and analysis of qualitative data for integrated maternal and child nutrition program planning. Atlanta, GA: CARE.
Infant & Young Child Nutrition (IYCN) Project. (2011). The basics: planning for formative research for infant and young child feeding practices [PDF, 253KB]. Washington, DC: USAID.
IYCN Project. (2012). Guidance for formative research on maternal nutrition. Washington, DC: USAID.
Pan American Health Organization. ProPAN Process for the Promotion of Child Feeding - A tool to improve infant and young child feeding.
Evidence of Effective, At-scale Nutrition SBCC
Alive & Thrive. (2013). Special issue of the food and nutrition bulletin. Food & Nutrition Bulletin 34:3 (Supplement).
Fabrizio, C. S., van Liere, M., & Pelto, G. (2014). Identifying determinants of effective complementary feeding behaviour change interventions in developing countries. Maternal and Child Nutrition 10(4):575–92.
Journal of Health Communication. (2014). Population-level behavior change to enhance child survival and development in low- and middle-income countries: a review of the evidence. Special Issue. Journal of Health Communication 19(1).
SPRING. (2014). Evidence of effective approaches to social and behavior change communication for preventing and reducing stunting and anemia: findings from a systematic literature review. Arlington, VA: SPRING.
SPRING. (2015). Designing the future of nutrition SBCC: how to achieve impact at scale. Conference Report and Strategic Agenda. Arlington, VA: SPRING.
References
Black, R. E., Victora, C. G., & Walker, S.P., et al. (2013). Maternal and child undernutrition and overweight in low-income and middle-income countries. The Lancet, 382(9890), 427–51.
Coates, J., & Galante, T. (2015). Agricultural commercialization, production diversity and dietary diversity among smallholders in Ethiopia: results from a 2012 National Integrated Agriculture and Socio-Economic Survey [PDF, 1.1MB]. Paper presented at the 5th annual Leverhulme Centre for Integrative Research on Agriculture and Health (LCIRAH) Conference, London, June 3, 2015.
Herforth, A., Jones, A., & Pinstrup-Andersen, P. (2012). Prioritizing nutrition in agriculture and rural development: guiding principles for operational investments. Health, Nutrition, and Population (HNP) Discussion Paper. Washington, DC: International Bank for Reconstruction and Development/World Bank.
The Lancet. (2013). Executive summary [PDF, 2.2MB]. Maternal and Child Nutrition Series.
Olney, D. K., Dillon, A., Pedehombga, A., et al. (2015). Integrated agriculture and nutrition programs can improve women's and children's nutritional status: evidence from Helen Keller International's Enhanced-Homestead Food Production Program in Burkina Faso [PDF, 1.1MB]. Paper presented at the 5th annual Leverhulme Centre for Integrative Research on Agriculture and Health (LCIRAH) Conference, London, June 3, 2015.
Strengthening Partnerships, Results, and Innovations in Nutrition Globally (SPRING). (2014a). Evidence of effective approaches to social and behavior change communication for preventing and reducing stunting and anemia: findings from a systematic literature review. Arlington, VA: SPRING.
SPRING. (2014b). Improving nutrition through agriculture technical brief series: understanding the women's empowerment pathway. Arlington, VA: SPRING.
SPRING. (2014c). SBCC pathways for improved maternal, infant, and young child nutrition practices. Arlington, VA: SPRING.
SPRING. (2015). Designing the future of nutrition SBCC: how to achieve impact at scale. Conference Report and Strategic Agenda. Arlington, VA: SPRING.
United Nations Children's Fund (UNICEF). (1990). Strategies of improving nutrition of children and women in developing countries. New York: UNICEF.
UNICEF. (2013). Improving child nutrition: the achievable imperative for global progress [PDF, 5.8MB]. New York: UNICEF.
U.S. Agency for International Development (USAID). (2014). Multi-sectoral nutrition strategy 2014–2025 [PDF, 1.3MB]. Washington, DC: USAID.
Webb, P., & Kennedy, E. (2014). Impacts of agriculture on nutrition: nature of the evidence and research gaps." Food and Nutrition Bulletin 35(1), 126–32.
World Bank. (2015). World development report 2015: mind, society, and behavior. Washington, DC: World Bank.
World Health Organization (WHO). (2013). Essential nutrition actions: improving maternal, newborn, infant, and young child health and nutrition. Geneva: WHO.
WHO. (n.d.). E-Library of evidence for nutrition actions. Geneva: WHO.
Footnotes
1. These are women's dietary diversity score; prevalence of exclusive breastfeeding of infants 0–5 months; prevalence of minimum acceptable diet of children 6–23 months; and number of HIV-positive, clinically malnourished clients who received therapeutic and supplementary feeding.
2.Prevalence of low birthweight and prevalence of moderate and severe hunger.
3. For evidence on effective at-scale nutrition SBCC, please see Additional Resources.
4. These include the MIYCN practices prioritized in The Lancet's 2008 and 2013 Maternal and Child Nutrition Series, WHO's "Essential Nutrition Actions" document (2013), WHO's e-Library of Evidence for Nutrition Actions, and the UNICEF 2013 report, "Improving Child Nutrition: The Achievable Imperative for Global Progress".
5. SPRING compiled the evidence for the positive relationship between each practice and nutritional status in a working paper: "SBCC Pathways for Improved Maternal, Infant, and Young Child Nutrition Practices" (SPRING, 2014a).
6. USAID's 2015 "WASH and Nutrition Implementation Brief" includes evidence for WASH's impact on nutrition and guidance for integrating WASH into nutrition and agriculture programs. Available at www.usaid.gov/what-we-do/global-health/nutrition/water-and-development-s....
7. For example, see the programming fundamentals highlighted in USAID's "Intensive Nutrition Programming Technical Guidance Brief" (2015).
8. Designers should use formative research to determine if improved behaviors are feasible. Assumptions about feasibility made by outsiders are often wrong. Factors that affect behaviors' feasibility include whether they are one time only or ongoing, frequent or infrequent, require one or many steps, require special skills, show immediate benefits, involve cost, require a lot of time, fit with social norms and identity, require goods and services that are easily available, require special technology, and require one person or many people.
9. See Additional Resources at the end of this brief for a list of guides for designing, conducting, and analyzing the results of formative and consultative research.
10. Visit spring-nutrition.org/sbccstrategicagenda to view additional background documents, including the Designing the Future of Nutrition SBCC: How to Achieve Impact at Scale conference materials.







Comment
Make a general inquiry or suggest an improvement.