- What We Do
- Agriculture and Food Security
- Democracy, Human Rights and Governance
- Economic Growth and Trade
- Education
- Ending Extreme Poverty
- Environment and Global Climate Change
- Gender Equality and Women's Empowerment
- Global Health
- Water and Sanitation
- Working in Crises and Conflict
- U.S. Global Development Lab

How one study's multilayered intervention approach may reduce this harmful barrier
March 2017 – By all accounts, the West African country of Senegal seems to have controlled its HIV and AIDS epidemic, as statistics show HIV prevalence as low as 0.5 percent among adults aged 15–49 in 2015,1 but this statistic does not tell the full story. While Senegal may seem to have low HIV numbers overall, HIV prevalence among key populations – particularly men who have sex with men (MSM) and female sex workers (FSW) – remains very high at nearly 41 percent.2 The difference between these numbers is largely due to an all too common negative factor: stigma. One study, however, is examining a combination intervention approach that shows strong potential in lessening this harmful barrier and thus increasing uptake in HIV services among these key populations.

Currently being implemented in three Senegal districts (Dakar, Mbour and Theis), the U.S. Agency for International Development (USAID), through the U.S. President's Emergency Plan for AIDS Relief (PEPFAR), is funding the HIV Prevention 2.0 (HP2) study. The study is made up of 172 MSM and 185 FSWs and is designed to develop and evaluate the impact of a multi-tiered integrated stigma mitigation intervention (ISMI) approach to optimizing HIV service delivery for key populations. The ISMI approach was made up of three interventions: 1) the pre-clinical, community intervention targeting perceived stigma; 2) the clinical intervention targeting enacted stigma in the healthcare settings; and 3) the web-based, post-clinical intervention aiming to increase diffusion of key population-friendly services and decrease perceived stigma.
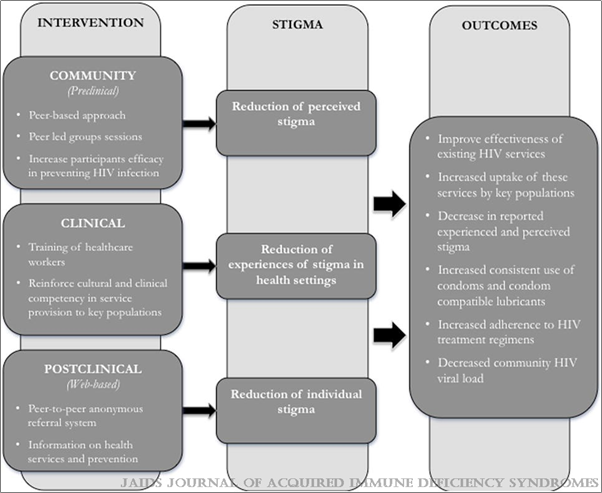
Perceived stigma refers to participants feeling afraid to seek or avoiding seeking healthcare services because they are worried someone may find out about their key population status. Enacted stigma refers to participants being denied or prevented from receiving healthcare services and/or hearing healthcare workers making discriminatory remarks about them because of their key population status. The ISMI approach is working to eliminate both types of stigma by implementing specific measures within the three interventions of its design (see Figure 1). For instance, the community intervention consists of peer-led group sessions to increase efficacy in preventing HIV infection. The clinical intervention consists of training healthcare workers and reinforcing cultural and clinical competency in service provisions for key populations. And lastly, the post-clinical intervention consists of an anonymous peer-to-peer referral system and information on health services and prevention.
An early assessment with the HP2 study cohort was conducted, in which researchers measured the difference between perceived and enacted (actual) stigma over the initial 6-month period since the study's start. Overall, both MSM and FSWs felt a significant decrease in perceived stigma. The percentage of FSWs who said they felt afraid and avoided seeking healthcare services because of perceived stigma decreased by roughly half. Similarly, nearly 10 percent (compared to the initial 17.7 percent) of MSM said they felt afraid to seek healthcare services because of perceived stigma, while close to 12 percent (compared to the initial 15.3 percent) of MSM said they avoided seeking healthcare services because of perceived stigma. Although the 6-month assessment did not see significant change in enacted stigma, the notable change in perceived stigma does show promise for the ISMI approach.
Stigma is a broad, and arguably, hard to describe term, yet it is commonly identified as one of the main drivers of high HIV prevalence, particularly among key populations. USAID, through PEPFAR, has a long history of working with community-based organizations to address stigma in HIV services and stigma mitigation remains integral to the agency's many programs. The early findings presented in the HP2 study on the multilayered ISMI approach leaves much to be optimistic about in eliminating stigma in HIV-related services, not only among MSM and FSWs in Senegal, but also for key populations across the globe.
Additional Links
- Potential Impact of Integrated Stigma Mitigation Interventions in Improving HIV/AIDS Service Delivery and Uptake for Key Populations in Senegal
- HC3 Webinar Presentation: Potential Impact of Integrated Stigma Mitigation Interventions in Improving HIV/AIDS Service Delivery and Uptake for Key Populations in Senegal
- Journal of Acquired Immune Deficiency Syndromes (JAIDS)
Footnotes
- www.unaids.org/en/regionscountries/countries/senegal
- 2014 data on HIV prevalence in men who have sex with men: www.aidsinfoonline.org/kpatlas/#/home







Comment
Make a general inquiry or suggest an improvement.