- What We Do
- Agriculture and Food Security
- Democracy, Human Rights and Governance
- Economic Growth and Trade
- Education
- Ending Extreme Poverty
- Environment and Global Climate Change
- Gender Equality and Women's Empowerment
- Global Health
- Water and Sanitation
- Working in Crises and Conflict
- U.S. Global Development Lab


Samantha Luffy, MPH
Program Analyst, HIV Vaccines
Recent Blog Posts
- Q & A with the New OHA Director Doug Arbuckle
OHA Communications - September 21, 2016 - Got Tang? A Blog Post to Honor David Stanton
OHA's Research Division - August 31, 2016
Every September, during Gynecological Cancer Awareness Month, the U.S. Agency for International Development (USAID) recognizes and remembers all who have been affected by cervical, ovarian, uterine and other forms of gynecological cancer. As development professionals dedicated to creating an AIDS-free generation, we are particularly humbled by cervical cancer's devastating statistics: cervical cancer hits hardest in low- and middle-income countries, and it is the most common type of cancer among women in sub-Saharan Africa. Caused by the human papilloma virus (HPV), it increases women's vulnerability to HIV acquisition. The result? Women living with HIV are four to five times more likely to develop cervical cancer than their HIV-negative peers.
Thankfully, there is an effective solution: if HIV-positive women receive cervical cancer screening, 80 percent of cases can be prevented [PDF, 851KB]. However, many women in sub-Saharan Africa, particularly those in high HIV-burden settings, do not receive regular screenings and are therefore at higher risk of developing cervical cancer.
To address this gap, USAID, through the U.S. President's Emergency Plan for AIDS Relief (PEPFAR)-supported Implementation Science Annual Program Statement (APS), supported Population Service International (PSI) in evaluating the effectiveness of integrating family planning and HIV services in Zambia. One of the main objectives there was to determine whether a low-cost, provider-initiated counseling and referral model with client follow-up increased women's uptake of add-on services like cervical cancer screening among women. Two enhanced service delivery models were compared against the standard of care in public clinics. Both enhanced service delivery models contained the following elements:
- A health-needs assessment and customized referrals during routine appointments with healthcare providers
- Follow-up phone calls 1 week after the participant's appointment to encourage uptake of cervical cancer screening
In addition to including all of the elements from the first model, the second enhanced service delivery model offered women an escort to their cervical cancer screening appointment.
Women seen by providers in both of the two enhanced service delivery models were five times as likely to receive cervical cancer screening at 6 weeks, and two times as likely to be screened as women receiving the standard of care at 6 months. In other words, more women who engaged with either of the enhanced service delivery models received more cervical cancer screenings than those who received the standard of care.
These results suggest that improving the linkage between cervical cancer screening with other health services, like family planning and HIV counseling and testing, is a feasible and cost-effective way to connect women at high risk of both HIV and cervical cancer to life-saving testing and screening, as seen below in Figure 1.
Figure 1. From Evidence to Action: Cervical Cancer Screening Among Women in Zambia.
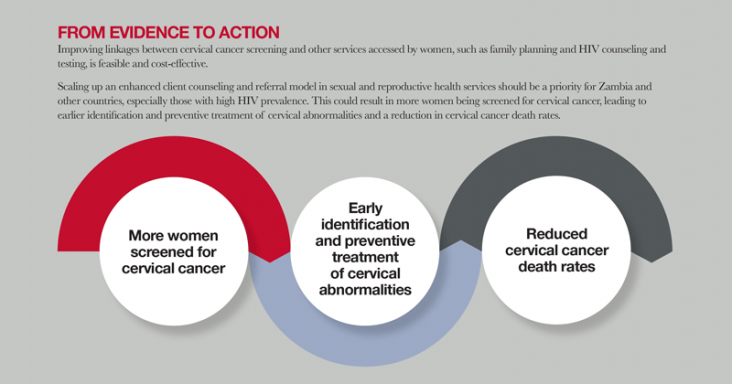
You can read the full story of the study's cervical cancer screening results in the new graphic brief here [PDF, 717KB]. The graphic brief – developed in collaboration with Project Supporting Operational AIDS Research (SOAR) – was designed to help policymakers and program designers promote the integration of two life-saving procedures: HIV testing and cervical cancer screening. Doing so could result in more women being screened for cervical cancer and, therefore, a reduction in cervical cancer death rates – an optimistic note to end on as we conclude Gynecological Cancer Awareness Month.
Principal Investigators Drs. Mutinta Nalubamba and Paul C. Hewett, along with skilled project staff at PSI, led the discovery of these important results through the PEPFAR-supported study, "Randomized Evaluation of Family Planning and HIV Service Linkage and Integration Models for Implementation at Scale in Zambia," 1 of 10 studies funded through the USAID Implementation Science APS. The graphic brief [PDF, 717KB] highlighting the key result was designed and developed in collaboration with another study by Project SOAR, which has a mandate to increase the use of data generated by PEPFAR-funded research. Results from this study, if effectively applied more broadly, could help protect women around the world from cervical cancer and HIV acquisition.







Add new comment