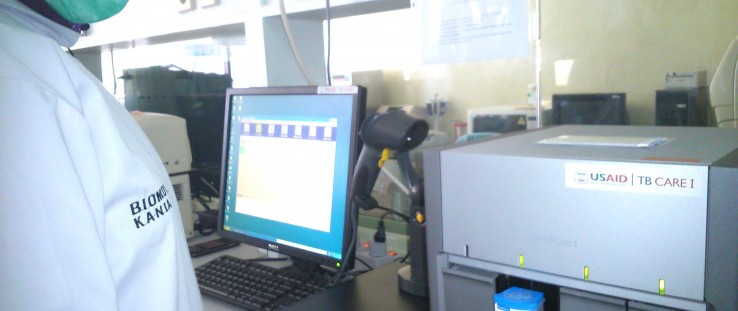
 The GeneXpert machine in use in Indonesia
Hasan Sadikin Hospital
The GeneXpert machine in use in Indonesia
Hasan Sadikin Hospital
 The GeneXpert machine in use in Indonesia
Hasan Sadikin Hospital
The GeneXpert machine in use in Indonesia
Hasan Sadikin Hospital
Muhajir remembers clearly the day one year ago when he made the eight-hour long journey from his rural home in Lampung, Indonesia, to a Jakarta clinic—a trip that probably saved his life.
A busy father of three children, Muhajir, who like many Indonesians only uses one name, worked as a high school teacher until he started experiencing symptoms of chronic fatigue and coughing, lost almost 50 pounds and had to quit his job. After years of ineffective treatments, he was referred to Jakarta’s Persahabatan Hospital, where he was finally correctly diagnosed with a multidrug-resistant strain of tuberculosis (MDR-TB)—one of more than 6,000 Indonesians who the World Health Organization (WHO) estimates suffer from MDR-TB each year.
At Persahabatan Hospital, the head of pulmonology medicine, Dr. Erlina Burhan, was able to quickly diagnose Muhajir’s MDR-TB and immediately placed him on medication.
Burhan considers Muhajir to be one of the lucky ones because he received a correct diagnosis and treatment regimen, which was made possible with new rapid diagnosis technology called GeneXpert. USAID is supporting the introduction of this new tool throughout Indonesia.
New Tool Brings New Hope
Developed through a public-private partnership between California-based Cepheid Inc., the Foundation for Innovative New Diagnostics, the University of Medicine and Dentistry of New Jersey, and the National Institutes of Health, the GeneXpert device dramatically reduces the lengthy diagnosis period for patients—from two months to as little as two hours. Patients can immediately start treatment, thereby preventing spread of the disease and saving lives.
“I was very frustrated in my early years as a pulmonologist,” says Burhan. “As clinicians, we knew from a physical examination and an analysis of symptoms that patients most likely had contracted a strain of multidrug-resistant TB, but we couldn’t do anything about it because we had to send the sample to a regional or national laboratory and wait months for a culture result. This slow diagnosis not only prolonged the patient’s suffering, but it also increased the chances of a patient dying before starting the appropriate treatment, not to mention an increased risk of spreading the disease in the community.”
Now with GeneXpert technology, health care workers simply insert a test cartridge containing a patient’s sputum (spit and phlegm) sample into the machine and wait for it to run its tests. The machine detects DNA sequences specific for tuberculosis and multidrug-resistant tuberculosis, then quickly analyzes data to produce very easy to understand results that doctors use to diagnose patients.
In December 2010, WHO began recommending using GeneXpert to diagnose TB, including in cases of HIV co-infection and multidrug-resistant strains. Recognizing the potential of this game-changing technology, USAID launched a series of activities and partnerships to enable and expand its use in developing countries.
In 2012, USAID began introducing GeneXpert to clinics in Southeast Asia, including Indonesia. In collaboration with the U.S. Centers for Disease Control and Prevention and the U.S. President’s Emergency Plan for AIDS Relief (PEPFAR), USAID is building on this tool in countries including Zimbabwe, Nigeria and South Africa to detect other infectious diseases such as HIV. There are also test cartridges available for influenza and human papilloma virus (cervical cancer)—both major issues in low- and middle-income countries.
“GeneXpert is the most exciting innovation in TB diagnostics in over a century,” says Amy Piatek, senior TB technical adviser for USAID’s Global Health Bureau. “It has the potential to significantly increase TB case detection in two priority populations in which traditional diagnostics are woefully inadequate—people with suspected HIV-associated TB and MDR-TB. The possibility to diagnose TB in these important groups in two hours will lead to fewer deaths and less transmission of disease.”
A Global Battle
Tuberculosis is a respiratory disease that is easily spread. In 2013, 9 million people contracted tuberculosis and 1.5 million died from the disease, according to WHO. The largest number of new TB cases occurred in the Southeast Asia and Western Pacific regions, accounting for 56 percent of new cases globally.
Globally, it is estimated that 5 percent of TB patients have a drug-resistant form of the disease. Drug-resistant TB treatment is much more difficult, lengthy and costly to treat. And it is much more fatal.
Since the 1880s, TB has been diagnosed through an examination of sputum under a microscope. For many decades, the diagnosis of drug-resistant TB has relied on complex techniques that involve growing TB bacterium from sputum—a slow process requiring sophisticated labs. Patients have to wait two or more months before receiving results and starting treatment, vastly increasing the chances an infected patient will transmit the airborne disease.
Strengthening tuberculosis programs in the countries with the highest burden, such as Indonesia, is essential to reducing TB locally and globally. Indonesia has struggled to combat TB for several decades. Every year, there are an estimated 500,000 new TB cases and approximately 64,000 TB-related deaths, with cases of highly contagious—and fatal—MDR-TB on the rise.
A Game Changer
Turning the tide on TB is one of the key health priorities identified under the U.S.-Indonesia Comprehensive Partnership, launched in late 2010 by Presidents Barack Obama and Susilo Bambang Yudhoyono to enhance cooperation between the two countries. Each year since 2011, USAID spends $13 million in Indonesia on detecting TB, ensuring patient treatment and improving the overall quality of patient care, working in close collaboration with Indonesia’s National Tuberculosis Program. These efforts have resulted in thousands of people being diagnosed and placed on treatment with an 86 percent success rate, which means Indonesia will meet its MDG goal for TB treatment. The majority of those treated are cured.
Around the world, there are now over 7,500 GeneXpert systems combatting the spread of tuberculosis, including over 3,500 installed in 110 high burden developing countries, according to Cepheid. What has helped drive the widespread adoption of this new diagnostic is an agreement announced in 2012 between USAID, PEPFAR, UNITAID and the Bill & Melinda Gates Foundation to subsidize the cost for countries in need through 2021. Under the agreement, GeneXpert test cartridges cost $9.98 (down from $16.86), and the most commonly used system to administer the test costs $17,000 (down from $78,000) for high-burden TB countries. The agreement has helped enable the purchase of approximately 3 million test cartridges during its first two years alone.
Saving Lives in Indonesia
Since introducing the devices to Indonesian medical facilities, the number of individuals with multidrug-resistant TB beginning treatment within one week of diagnosis has increased from 2 to 18 percent. The use of GeneXpert in Indonesia has drastically decreased the number of days a patient has to wait between diagnosis testing and beginning treatment—from an average of 81 to only 15 days. There has also been a significant decrease in mortality of multidrug-resistant TB patients during the diagnostic process.
Persahabatan Hospital was one of the first facilities to receive GeneXpert, and Burhan says the impact has been dramatic. “As a clinician, I’m very happy with [GeneXpert] because I can treat a multidrug-resistant TB patient as soon as they are diagnosed without delay, and stop them from transmitting TB to others.”
In addition to its speed in delivering results, the GeneXpert device is compact and can fit on a small table. Hospital laboratory technicians report that it is very easy to use. The device was designed to be used at the local level, in simpler facilities that cannot process bacterial cultures.
Another patient, Lily, a 37-year-old mother of three young children from North Jakarta, was diagnosed with multidrug-resistant TB following a GeneXpert test in August 2014. Lily, who like Muhajir uses only one name, was immediately placed on a treatment plan by doctors.
Lily, who makes her living by selling coffee from a street kiosk, struggles to both raise her three children and pay for the $3 a day trip to the hospital to get her treatments (provided free of charge by the government). But she is willing to make the sacrifice for the sake of her family. “I don’t [worry about] the money as long as I can be cured so I can raise my children,” she says.
While TB can infect anyone, regardless of their socioeconomic level, poor people are more vulnerable due to poor nutrition, overcrowding and challenges accessing medical services.
Successfully treating people with multidrug-resistant TB takes two years or more, and there are often difficult side effects to manage. “Though drug-resistant TB is a health problem, it needs comprehensive management, not only from the patient’s side but also from the health provider and government,” said Burhan.













Comment
Make a general inquiry or suggest an improvement.